Psychiatric disorders are a group of mental illnesses that disturb an individual’s mood, thinking, and behavior, and they represent an important health concern in today’s society. In 2018 alone, 19% of US adults (47.6 million) experienced mental illness, representing 1 in 5 adults. Anxiety disorders are the most common subtype of psychiatric disorder among American adults, with a prevalence of 18.1%, followed by major depression at 7.2%. Depression is the leading cause of disability in both males and females worldwide, and it is estimated that depression and anxiety disorders cost the global economy $1 trillion in lost productivity each year.
The most common treatment for mental illnesses is medication (e.g., antidepressants and antipsychotics). Psychotherapy is often useful in the treatment of mental illness as well and there are many different types of therapy (e.g., cognitive behavioral therapy and interpersonal therapy) that can be beneficial for recovery. Although these modalities work well for a majority of patients, there is a subset suffering from treatment-resistant disease.
Treatment-resistant mental illness is defined as a condition that fails to respond to two or more medication therapies. The more severe treatment-resistant psychiatric conditions, such as depression, have been associated with high rates of suicide and disability. An increased recognition of the seriousness and burden of psychiatric diseases, has led to a corresponding increased need for the development of safe and effective surgical interventions for the management of patients with treatment-resistant psychiatric disorders.
Interestingly, psychosurgery, or the neurosurgical treatment of mental disorders, has been practiced since 1936 when neurologist António Egas Moniz began treating certain psychoses with frontal lobotomies, which involved severing neural connections in the brain’s prefrontal cortex. This procedure was very popular in the 1940’s and 1950’s. Due to severe side effects, such as worsened mental illness and major personality change, this procedure was abandoned; however, newer, less destructive, and more precise neurosurgical procedures for the treatment of mental disorders have been established.
Surgical interventions, such as deep brain stimulation (DBS) and ablative brain lesioning via radiofrequency ablation or gamma knife radiosurgery, have shown moderate success in the treatment of treatment-resistant mental illness. These procedures target precise locations within different brain structures that are involved in the pathophysiology of psychiatric disease. Given its safety and noninvasiveness, focused ultrasound thermal ablation or neuromodulation of these targets could offer a more attractive treatment alternative to DBS, radiofrequency ablation, or gamma knife radiosurgery.
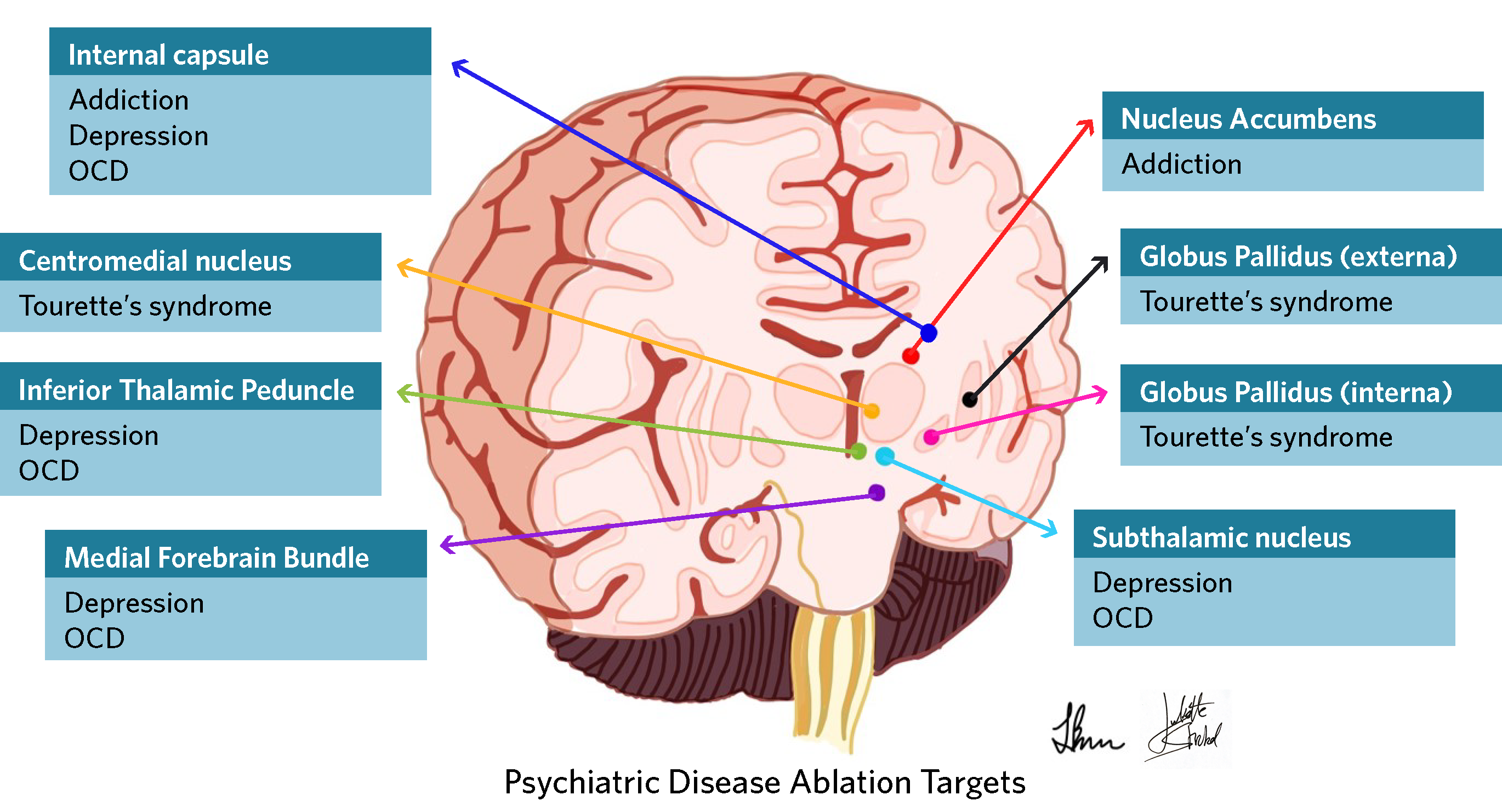
The following is an overview of psychiatric disorders for which focused ultrasound could be used as a therapeutic option in severe or treatment-refractory cases. The novel use of the technology to treat obsessive-compulsive disorder (OCD), major depression, and even addiction are currently being investigated in clinical trials described below. In addition, focused ultrasound holds promise for treating anorexia nervosa, aggression and disruption, and Tourette’s syndrome.
Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder (OCD) can significantly interfere with activities of daily living, causing extreme anxiety and stress to those afflicted by this mental disorder. OCD has an annual prevalence of 1.2% in the United States (estimated 3 million people). Obsessions are defined as recurrent and persistent thoughts while compulsions are repetitive physical behaviors (hand washing) or mental acts (praying). Patients with OCD have symptoms that disrupt even simple routines and often have difficulty tolerating uncertain situations. Recently, the World Health Organization ranked OCD in the top 10 most disabling illnesses by lost income and decreased quality of life; and it is in fifth position for women aged 15-44 years. Importantly, 90% of patients diagnosed with OCD will suffer from another psychiatric disorder, such as anxiety, impulse control disorders, and substance abuse. Although the majority of patients respond to conventional treatment such as medication and behavioral therapy, up to 33% of patients are treatment resistant and manifest decreased social and occupational functioning.
In these more severe cases, ablative surgery of specific brain regions using radiofrequency ablation and stereotactic radiosurgery have yielded varying response rates. Because the underlying etiology of OCD is complex and involves multiple neuronal circuits, varying target sites for ablation have been explored to disconnect abnormal circuitry, including the anterior limb of the internal capsule and the anterior cingulate gyrus. A review article that examined the use of either radiofrequency ablation or gamma knife radiosurgery to ablate bilateral targets in the anterior limb of the internal capsule (anterior capsulotomy) found that these techniques achieved a 51% mean reduction in symptom severity. Because radiofrequency ablation is an invasive procedure wherein electrodes are guided through the brain to the target area, it carries risks such as infection and bleeding. Although gamma knife radiosurgery is noninvasive, its disadvantages include the use of ionizing radiation and a long latency period of weeks to months to obtain a clinical response. DBS has also been used for treatment-resistant OCD, but again involves invasive neurosurgery with insertion of electrodes into the brain which then requires continuous monitoring, adjustment of electrodes, and substantial costs to the patient that may not covered by insurance.
Comparatively, magnetic resonance-guided focused ultrasound (MRgFUS) therapy is noninvasive and does not use ionizing radiation. Its immediate thermal effects confirm ablation of the desired target during the procedure. A recent study published by researchers at Stanford University found MRgFUS to be a more cost-effective treatment than radiofrequency ablation due to its noninvasive nature and low rate of complications. MRgFUS may also mitigate the uncertainties (often not tolerated by patients with OCD) associated with invasive procedures like radiofrequency ablation or DBS.
Science Highlight
The first in human trial of MRgFUS for OCD occurred in four patients in Korea and reported a 33% improvement in symptom severity (Y-BOCS score) over six months with significant improvement in mood (61%) and anxiety (69%). Additional studies published comparable results that were durable at the two-year follow up. Following a similar treatment protocol, the first trial in North America is currently recruiting patients at Sunnybrook Health Sciences Centre in Toronto. Five out of ten patients have already been enrolled, and the study is expected to complete enrollment by the end of 2019.
In collaboration with the Focused Ultrasound Foundation, a team of researchers recently received positive feedback during an in-person FDA pre-submission meeting regarding the future approval of a clinical study to evaluate MRgFUS for OCD in the United States. The unique protocol design was developed by a steering committee comprised of experts in the field, led by neuropsychiatrists Renana Eitan, MD, from Brigham and Women’s Hospital and Mahendra Bhati, MD, from Stanford University. The protocol ensures best medical treatment for patients with OCD while incorporating both treatment and sham arms with subsequent cross over.
HEAR FROM AN EXPERT
 Renana Eitan, MD, Functional Neuroimaging Laboratory, Brigham and Women’s Hospital
Renana Eitan, MD, Functional Neuroimaging Laboratory, Brigham and Women’s Hospital
“Despite their high prevalence, social impact, and variety of therapeutic options for OCD and depression, many patients remain treatment-resistant. For these severely ill patients who do not respond to psychotherapy and medication, advanced brain stimulation techniques should be prescribed. In the past, ablative procedures such as anterior capsulotomy and cingulotomy had been associated with a high success rate in the most severe and treatment resistant patients, although they are now infrequently used due to potential side effects and the irreversibility of the treatment. Focused ultrasound therapy offers the possibility of safer brain lesioning, in part by eliminating the need for open surgery or an invasive procedure. There is no radiation, incisions, burr holes, and lesions are generated in real-time under MR image guidance. Focused ultrasound represents a simple and cost-effective treatment plan for depression and OCD patients.
Future applications of focused ultrasound might include reversible and adjustable neuromodulation of brain circuits that are relevant to psychiatric disorders. Reversible focused ultrasound neuromodulation can assist in the identification of new brain targets for the treatment of severe psychiatric disorders, such as the negative symptoms of schizophrenia.”
Major Depression
Major depressive disorder (MDD) is a serious medical illness that can interfere with activities of daily living, thoughts, and actions. Common symptoms include feelings of sadness or loss of interest, loss of self-esteem, changes in appetite, trouble sleeping, and thoughts related to death or suicide. These symptoms can range from mild to severe and must last at least two weeks to qualify as a diagnosis.
The most common treatment for MDD is medication, but 50% to 66% of patients do not fully respond to antidepressant therapy alone. Those patients require additional interventions such as psychotherapy. For severe depression, electroconvulsive therapy is a treatment option that occurs while a patient is under anesthesia; although it can be highly effective, relapses are common. There remains a need for alternative therapies in individuals with treatment-resistant depression (TRD). Invasive surgeries, such as ablation of neural tracts and deep brain stimulation (DBS), are offered to this subset of patients. Current ablative modalities include radiofrequency ablation, laser ablation, or stereotactic radiosurgery (gamma knife or linear accelerator). Such surgeries may result in a 32% to 60% improvement in symptoms; however these procedures carry a risk of infection, bleeding, or exposure to harmful radiation. DBS is also being used in patients with TRD to electrically modulate specific areas in the brain that contribute to the pathogenesis of depression. Another noninvasive treatment, transcranial magnetic stimulation (TMS), is well tolerated and benefits approximately 50% to 60% of patients with TRD, but relapse is common and TMS does not treat a target area with high spatial resolution. Given the moderate success reported with other ablative therapies and DBS, focused ultrasound could provide a noninvasive, non-radiating, low-risk procedure with precise targeting abilities.
Science Highlight
A recent Emory University publication examined long-term outcomes after using DBS for TRD and reported sustained safety and efficacy over a treatment period of two to eight years. The brain stimulation target in this study was the subcallosal cingulate. Of 28 patients, 14 completed eight or more years of DBS and another 11 completed at least four years. Response to the therapy remained greater than 50%, and remission rates were maintained above 30% through years 2 to 8 of the follow-up period with 21% of all patients demonstrating continuous response to treatment from the first year onward. Although this study reports that invasive neuromodulation techniques to specific areas of the brain can result in durable success, newer noninvasive procedures to similar targets could provide similar results with less risk and at a lower cost.
A phase 1 trial of magnetic resonance-guided focused ultrasound (MRgFUS) bilateral anterior capsulotomy for the treatment of MDD is currently enrolling 10 patients at Sunnybrook Health Sciences Centre in Toronto. In this study, MRgFUS is being used to noninvasively ablate a target in the anterior limb of the internal capsule in order to disrupt a neural pathway involved in the pathogenesis of MDD. Thus far, five out of twelve patients have been treated. This trial will likely pave the way for similar studies to commence in the United States in 2020.
HEAR FROM AN EXPERT
 Nir Lipsman, MD, PhD, Sunnybrook Health Sciences Centre in Toronto, Canada
Nir Lipsman, MD, PhD, Sunnybrook Health Sciences Centre in Toronto, Canada
“We now recognize that common and challenging conditions, like depression and OCD, are driven by dysfunctional circuits in the brain. Advances like focused ultrasound can be used to influence those circuits and potentially reset them.”
Addiction
Addiction is defined as compulsive substance use despite harmful consequences. According to the American Addiction Centers, nearly 20 million Americans over 12 years of age had a substance abuse disorder in 2017. Those aged 18-25 suffer the most from this disease, representing 14.8% of the addicted population followed by adults >26 years of age (6.4% of the population) and even adolescents between 12 and 17 (4% of the population). The number of overdose deaths is especially concerning as there were over 72,000 deaths in 2017, of which 68% were due to opioids. On average, 130 Americans die every day from opioid overdose.
It is estimated that only 19% of patients with a substance abuse problem receive treatment, and relapse occurs in 40-60% of those who achieve successful recovery. Risk factors for developing an addiction include a positive family history of addiction, environmental factors such as early childhood exposure to drugs and alcohol, and underlying mental health disorders. Over $740 billion dollars are spent annually due to lost workplace productivity, healthcare expenses, and crime related costs secondary to addiction.
The abnormalities in addiction are related to dysfunction in the Mesolimbic reward system and involve circuits in the frontal lobe and deeper areas of the brain. Although invasive procedures such as cryoablation and radiofrequency ablation targeting of the frontal lobes and nucleus accumbens showed improvement in 60-65% of patients, these studies were halted due to their invasive nature and ethical concerns. A study of deep brain stimulation (DBS) for the treatment of addiction demonstrated improvement in pleasure seeking behaviors and resolution of drug addiction. These results led to more specific targeting of the nucleus accumbens and although the study groups were small in number and no randomized control studies were performed, patients reported decreased drug usage.
As there are multiple concerns regarding consent and risk of pain in performing invasive surgical procedures in patients with addictions, magnetic resonance-guided focused ultrasound (MRgFUS) could provide a noninvasive alternative that is attractive to patients, families, medical professionals, and our health care system. The one-time ablation of deep brain targets such as the nucleus accumbens with MRgFUS may allow for a more durable, long lasting effect that acts as a complement to existing medical and behavioral treatments for difficult to treat addictions.
Science Highlight
At the West Virginia University Rockefeller Neuroscience Institute (RNI), neurosurgeon Ali Rezai, MD, is leading the way to finding an alternative treatment for Opioid Use Disorder (OUD). Rezai’s team is examining the safety and efficacy of nucleus accumbens DBS in a feasibility trial for OUD. The RNI team has also demonstrated the use of repetitive transcranial magnetic stimulation (rTMS) of the prefrontal cortex in reducing the cravings for cocaine and heroin. The RNI team is now exploring the use of low-intensity MRgFUS to the nucleus accumbens to target the same areas of the brain in a noninvasive fashion.
HEAR FROM AN EXPERT
 Ali Rezai, MD, West Virginia University Hospital
Ali Rezai, MD, West Virginia University Hospital
“The reward circuitry of the brain is impaired in addiction and the Nucleus accumbens is a key structure in this network, and a target for neuromodulation. We are initiating a pilot feasibility study investigating the use of low intensity MRgFUS to modulate the nucleus accumbens to reduce cravings in opioid addiction.”
Anorexia Nervosa (AN) is defined as an extremely low body mass index (less than18.5kg/m2) accompanied by extreme fear and preoccupation related to weight and body image. It has a lifetime prevalence of 0.6%, affecting more females (0.9%) than males (0.3%) and the highest mortality rate of all psychiatric disorders.
Conventional treatments including behavioral, nutritional, and pharmacologic therapies have a disappointing, 50% failure rate. Due to the high treatment failure rate and consequent high mortality rate, other treatment options are necessary to save the lives of patients with AN. Neurosurgical ablative procedures have traditionally targeted the frontal lobe white matter, which controls cognitive skills, the anterior limb of the internal capsule, which connects the thalamus to the frontal lobe, and the nucleus accumbens which mainly affects the reward circuit. There are also studies using deep brain stimulation (DBS) to target these same areas. However, the use of stereotactic surgery to perform bilateral anterior capsulotomies has been limited due to its potential for irreversible side effects, including incontinence, sleep disorders, and fatigue. As for DBS, most patients with AN lack sufficient muscle and fat required for the necessary hardware to be implanted into the chest wall. Focused ultrasound could provide a safer, noninvasive, ablative treatment option for patients with AN.
Science Highlight
During the 2017 psychiatric disease workshop sponsored by the Focused Ultrasound Foundation, a group of psychiatrists, neurologists, and neurosurgeons agreed that the evidence in the literature supports initiating a trial with magnetic resonance-guided focused ultrasound targeting the anterior limb of the internal capsule.
Aggression and Disruption
Aggression and disruption is exhibited in behaviors that lead to damage or destruction of physical objects with some kind of objective and not necessarily provoked in the traditional manner. Disruptive behaviors may include throwing, kicking, and breaking objects. These behaviors increase the likelihood of causing injury to oneself and others as well as greatly impede an individual’s ability to function in a typical community. According to the Kennedy Krieger Institute, aggression increases with age, affects 2% to 20% of individuals with intellectual disabilities, and is often associated with comorbid mental illnesses that complicate treatment. The underlying pathophysiology of aggression is not fully understood, but is thought to be mediated in part by a complex neural circuit called the limbic system, which affects social and anxiety-like behavior. The limbic system connects various parts of the brain, such as the amygdala, which processes emotions.
First-line treatment for aggressive and disruptive behavior is with medication management. However, nearly a third of patients will not respond to initial treatment and often suffer from a myriad of side effects. For cases refractory to treatment, deep brain stimulation (DBS) may be an option.
Several reports describe improvement in aggressive behavior in patients treated with DBS for other comorbidities including autism and mental retardation. The targets for DBS in these studies included the nucleus accumbens and the posterior hypothalamus. Magnetic-resonance guided focused ultrasound (MRgFUS) may offer a less invasive means to achieve similar treatment outcomes in people who suffer from aggressive and disruptive behaviors.
Science Highlight
Further studies are evaluating the use of DBS and brain lesioning in patients with treatment refractory aggression. Similar targets may be suitable for noninvasive MRgFUS ablation or neuromodulation.
Tourette’s Syndrome
Tourette’s syndrome (TS) usually manifests in childhood as motor and/or phonic tics. Although tics gradually improve over time, nearly 25% of people may experience persistent symptoms that drastically impair quality of life and challenge their ability to maintain relationships with family and friends. Pharmacological therapy of TS focuses around dopamine depleting drugs but their use is restricted by long-term side effects including sedation, weight gain, hyperprolactinemia, Parkinsonism, and tardive dyskinesia.
Surgical intervention for TS is limited to deep brain stimulation (DBS), which has demonstrated improvement in symptom severity and quality of life. The two most common targets for DBS in TS are the thalamus, which relays motor and sensory signals to the cerebral cortex in the brain, and the Globus pallidus internus (GPi), which regulates voluntary movement. Similar targets could be used to treat TS with focused ultrasound instead of DBS.
Science Highlight
By translating preclinical ablative research and DBS studies, magnetic resonance-guided focused ultrasound could be investigated as a treatment modality to noninvasively ablate GPi or thalamus targets.
Conclusion
Focused ultrasound is a promising technology that could offer a safe, noninvasive treatment of a wide variety of psychiatric disorders. The benefits of focused ultrasound lie in its submillimeter precision targeting without incisions or exposure to ionizing radiation. Because there are significant decreased risks, perhaps more patients would consider focused ultrasound as a treatment alternative in medication-refractory cases. Clinical trials are already underway to examine the safety and efficacy of focused ultrasound for the treatment of OCD, depression, and addiction, and there is prime potential for this technology to noninvasively treat many other psychiatric disorders in the future.
HEAR FROM AN EXPERT
 Rees Cosgrove, MD, FRCSC, FACS, Brigham & Women’s Hospital
Rees Cosgrove, MD, FRCSC, FACS, Brigham & Women’s Hospital
“Neurosurgical interventions for patients suffering from severe, disabling, and completely treatment refractory major depression or OCD have been performed for many years with good success. The possibility of being able to reproduce these salutory outcomes with a less invasive procedure is very appealing and should be explored.”
References
Ruscio AM, Stein DJ, Chiu W, Kessler RC. The Epidemiology of Obsessive Compulsive Disorder in the National Comorbidity Survey Replication. Mol Psychiatry 2010;15(1):53-63.
Langevin JP. The amygdala as a target for behavior surgery. Surg Neurol Int 2012; 3(Supp1):S40-46.
Doshi PK, Hegde A, Desai A. Nucleus Accumbens (NAc) DBS for obsessive compulsive disorder and aggression in an autistic patient: a case report and hypothesis of the role of NAc in autism and comorbid symptoms. World Neurosurg 2019;125:387-391.
Jung HH, Kim SJ, Roh D, Chang JG, Chang WS, Kweon EJ, Kim CH, Chang JW. Bilateral thermal capsulotomy with MR-guided focused ultrasound for patients with treatment-refractory obsessive-compulsive disorder: a proof-of-concept study. Mol Psychiatry 2015;20(10):1205-11.
Franzini A, Broggi G, Cordella R, Dones I, Messina G. Deep-brain stimulation for aggressive and disruptive behavior. World Neurosurg 2013;80(3-4):S29.e11-24.
Thenganatt MA, Jankovic J. Recent Advances in Understanding and Managing Tourette Syndrome. F1000Res 2016;5.
Johnson KA, Fletcher PT, Servello D, et al. Image-based analysis and long-term clinical outcomes of deep brain stimulation for Tourette syndrome: a multisite study. J Neurol Neurosurg Psychiatry 2019;90(10):1078-1090.
Brito M, Teixeira MJ, Mendes MM, et al. Exploring the clinical outcomes after deep brain stimulation in Tourette syndrome. J Neurol Sci 2019;402:48-51.
Greenberg BD, Rauch SL, Haber SN. Invasive Circuitry-Based Neurotherapeutics: Stereotactic Ablation and Deep Brain Stimulation for OCD. Neuropsychopharmacology 2010;35(1):317-336.
Janicak PG, O’Reardon JP, Sampson SM, et al. Transcranial magnetic stimulation in the treatment of major depressive disorder: a comprehensive summary of safety experience from acute exposure, extended exposure, and during reintroduction treatment. J Clin Psychiatry 2008;69(2):222-232.
Kubu CS, Brelje T, Butters MA, et al. Cognitive outcome after ventral capsule/ventral striatum stimulation for treatment-resistant major depression. J Neurol Neurosurg Psychiatry 2017;88(3):262-265.
Dandekar MP, Fenoy AJ, Carvalho AF, Soares JC, Quevedo J. Deep brain stimulation for treatment-resistant depression: an integrative review of preclinical and clinical findings and translational implications. Mol Psychiatry 2018;23(5):1094-1112.
Kim M, Kim CH, Jung HH, Kim SJ, Chang JW. Treatment of Major Depressive Disorder via Magnetic Resonance-Guided Focused Ultrasound Surgery. Biol Psychiatry 2018;83(1):e17-e18.
Wang TR, Moosa S, Dallapiazza RF, Elias WJ, Lynch WJ. Deep brain stimulation for the treatment of drug addiction. Neurosurg Focus 2018;45(2):E11.
National Alliance on Mental Illness. Mental health by the numbers. Updated September 2019. Accessed October 15, 2019.
Thomas S. Alcohol and Drug Abuse Statistics. American Addiction Centers website. Updated July 29, 2019. Accessed September 15, 2019.
Mahoney JJ, Marshalek PJ, Rezai AR, Lander LR, Berry JH, Haut MW. A case report illustrating the effects of repetitive transcranial magnetic stimulation on cue-induced craving in an individual with opioid and cocaine use disorder. Exp Clin Psychopharmacol. 2019 Oct 24.
Crowell AL, Riva-Posse P, Holtzheimer PE, Garlow SJ, Kelley ME, Gross RE, Denison L, Quinn S, Mayberg HS. Long-Term Outcomes of Subcallosal Cingulate Deep Brain Stimulation for Treatment-Resistant Depression. Am J Psychiatry 2019 Oct 4.
